Nursing Education Models and Educator Role
Role of Nursing Educator
Instructors should carefully outline the specific objectives that are to be met in each laboratory session. Again, there should be a planning session in which this information is decided by a dedicated group of people. A curriculum committee may be charged with this task, or a task force set up for this purpose.
Further decisions need to be made about how the skills will be introduced, mastered, and evaluated. Generally, it is necessary for each program to have internal consistency. Policies regarding skill competencies need to be established throughout the entire program.
Every course does not need to be cookie cutter identical, but there does need to be congruency in what is presented in the LRC , and how it will be evaluated throughout the program. The activities that take place in the LRC can vary greatly from course to course and program to program. Many programs choose to introduce selected skills in a formal manner, with identified objectives and skill checklists.
A nursing faculty member in the course is
assigned to present the content to the students, and the students practice with
supervision and guidance. This may be the extent to which some skills are
introduced, or there may be a requirement to complete a formal testing process
to determine competence.
To facilitate the transition within nursing education to the practice doctorate by the target date of 2015, the AACN board created two task forces with representation from diverse nursing specialties and institutions.
The first task force was charged with creating an “Essentials” document for practice doctorates, which outlines the basic competencies that must be built into these educational programs. This document is similar in nature to the other Essentials documents originated by AACN for baccalaureate and master's degree education.
The second task force,
the road map task force, is focused on implementation of the new position
statement and issues related to this transition, including moving existing
Advanced Practice Nurse (APN) programs to the doctoral level and providing
efficient bridge programs for master's prepared nurses interested in pursuing a
DNP degree.
The Essentials document has a format similar to that of the AACN Essentials of Master's Education for Advanced Practice Nursing (AACN, 1996) and includes the core competencies for all DNP graduates. The specialty role competencies, an essential component of the DNP curriculum, will be identified by the specialty nursing organizations.
A diagram of the DNP curriculum, as currently envisioned. An individual may enter a DNP program following a baccalaureate nursing education program, a master's advanced generalist program such as a CNL program, or one of the current master's APRN programs.
Therefore, the DNP Essentials or end-of-program competencies include all of the post-baccalaureate nursing competencies necessary upon graduation from a practice doctorate in nursing program.
Following the transition to this new model of specialty
nursing education, it is possible that the current Essentials of Master's
Education may be retired, having been replaced by the new Essentials of the
Doctor of Nursing Practice and possibly a new set of guide lines for advanced
generalist education at the master's level.
New Model for Nursing Education
With the proposed future
changes in nursing education, a number of differing models are possible. One
such model for future nursing education and the entry points and pathways that
could be taken throughout the model are presented here.
Educational Pathways For the health of the profession, nursing must maintain a robust pipeline of entry level clinicians and provide seamless pathways to higher levels of educational achievement. Mechanisms must be strengthened to allow articulation or transition from one nursing degree program to another.
These pathways should ensure that individuals receive appropriate academic credit for previous education and clinical experiences, that appropriate course and credit requirements are assigned to appropriate degrees, and that program requirements are not redundant.
Ensuring these transition mechanisms also should standardize nursing education program expectations, including length of programs and ranges of credit and clinical requirements, and should improve access to the continuum of nursing education programs. Completion of each degree should be based on documentation of end-of-program competencies delineated in the Essentials for each degree (baccalaureate, master's, and doctoral).
This requires nursing,
just as the rest of higher education is doing, to examine and develop new
mechanisms for assessing outcome competencies, such as virtual testing,
simulations, and portfolio development (AACU, 2004).

Nursing Curricula Interfaces
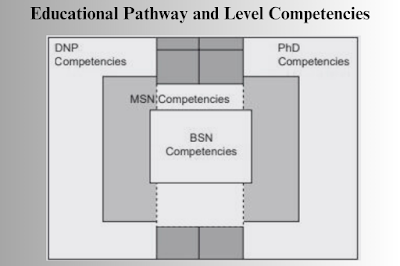
End-of-program competencies for the BSN, MSN, DNP, and PhD nursing programs are not discrete but overlap and build on each other. How each degree program curriculum, or end-of-program competencies, interlocks. The specific areas of overlap in competencies and content are dependent upon the individual's previous educational background and clinical experience.
For example, an individual who holds an MSN degree with preparation as a CNL or an APRN will already have attained many of the end-of-program competencies expected of the DNP graduate.
On the other hand, an individual who
enters the DNP program immediately after obtaining a BSN will need extensive
graduate level preparation in an advanced area of nursing practice. Likewise,
areas of overlap between the DNP and PhD curricula may exist, depending upon
the area of study, research, and practice.
Nurses, more than any other health professionals, have constant contact with patients and opportunities to influence outcomes of care. Nurses provide services across the continuum of settings from critical care, senior day care to school health facilities. The IOM and other well-respected interdisciplinary groups have urged all health professions to redesign the way future practitioners are prepared.
Current and projected changes in an increasingly complex health-care system, and the nursing profession's potential to influence health-care outcomes have created a powerful mandate to prepare a highly and differently educated future nursing workforce. Nursing also must participate in and lead the redesign of care delivery models.
New practice and education models are needed to attract highly qualified and professionally motivated individuals to the profession. This vision presented is just one possible model for future nursing education.
This model includes a minimum of a baccalaureate degree for entry into professional nursing practice, graduate level preparation in an advanced generalist role, doctoral preparation for practice in all nursing specialties, and research focused doctoral preparation to expand nursing knowledge and scientific base.
What may occur in the future cannot be predicted and will be dependent upon the nursing community as a whole. A future nursing education model requires an evolution and expansion of nursing education at all levels of practice. The nursing profession cannot afford to be the least educated profession at the health professions' table.
Nursing cannot rely on past
experiences and current practices. An open, thoughtful, and creative dialogue
is needed to achieve this new model of nursing education, for which the
ultimate goals are an expanded highly educated nursing workforce, increased
access to high-quality care, and improved health-care outcomes. Previous




Give your opinion if have any.